Digital health technologies are critical infrastructure and enablers for high quality, equitable health outcomes. Since the publication of PwC’s 2022 Digital Health Trends there has been significant change in Aotearoa New Zealand’s digital health space.
In the public sector, Te Whatu Ora and Te Aka Whai Ora are now in operation and the Ministry of Health’s Data and Digital Directorate has transitioned to Te Whatu Ora. Shared service providers such as healthAlliance and TAS Kāhui Tuitui Tāngata are also now part of Te Whatu Ora. Meanwhile, across the private digital health sector, industry and healthcare organisations are investing in innovative solutions. In doing so these organisations continue to strive for more equitable, connected, and efficient service offerings. There is also emerging competition for demonstrating connectedness and information sharing.
We also saw the 2022 Interim New Zealand Health Plan provide some certainty and direction to the digital health sector. The Government has signalled its intention to bring a national approach to digital solutions, aiming to improve the capacity of services for digitally-enabled service delivery, increasing digital access options and improving digital literacy.
Meanwhile, as COVID-19 moves from pandemic to endemic, many organisations need to revisit and renew their digital health strategies. Some organisations will aim to strategically capitalise and scale from the investment and rapid deployments of the last few years, while others – influenced by the increasing number of cyber attacks – will strategically invest in enhancing organisational cybersecurity.
PwC’s Digital Health Trends 2023 is set against the backdrop of these contextual and emotive environmental factors.
Four key digital health trends 2023

People and whānau: nothing about us, without us
Over the next 12 months we expect to see more consumer involvement in the co-design of digital solutions, which will really give power to the phrase ‘nothing about us, without us’. This year the National Clinical and Consumer Health Design Council1 will commence meeting, giving consumer representatives more seats at the decision-making table.
As a result of genuine co-design, with people and whānau at the centre, the digital health agenda will shift beyond a traditional clinical healthcare focus to a more holistic, whole person, approach. For the market, this will drive the implementation of customer relationship management (CRM) solutions, particularly in the NGO sector where vulnerable communities and equity concerns require a more holistic view of individuals and whānau. We expect the bridging of social, well-being, education, and health sectors will be demonstrated by NGO and private partnerships.
We’ve already seen the benefits of this approach with Te Hau Ora o Ngāpuhi’s innovative Service Management System2, which captures information on whānau, and whakapapa and provides a holistic view of whānau relationships and the wider community. Understanding the needs and background of whānau has allowed Te Hau Ora o Ngāpuhi to better determine the support services required to achieve long-term benefits for the whole community.
Collaboration is the key word through the continuation and expansion of social service provider partnerships, where digital becomes crucial in sharing information. Both globally and domestically there is a concerted effort to develop and implement the FHIR standard for the International Patient Summary (IPS). The IPS comprises data elements that have the potential to provide high value across countless clinical and wellbeing workflows. To further deliver to people and whānau we’ll likely see renewed interest in standards development, and the IPS as the vehicle for sharing information across the health and social continuum.
The extent to which private and public solutions are able to secure funding to scale their solutions will be dependent on additional investment in measurement and evaluation of their implementations – generating evidence of impact on equity and health outcomes.

Leadership: brave and bold leaders needed to drive progress
To progress Aotearoa New Zealand’s digital maturity requires leadership that can challenge the status quo, break legacy ways of working and shift mindsets entrenched in the past. The future digital health leaders have to be ambitious, and able to garner widespread support and funding. They have to be able to pick up the pace of transformation while demonstrating empathy during a transformational shift. Digital health leaders need to communicate and collaborate confidently and effectively with peak clinical and industry leaders, iwi and Ministers, and across all levels of the health workforce.
Our collective imperative to demonstrate improvements in equity and health outcomes requires brave leadership, and the reforms of the last three years have been hugely disruptive to the health sector’s tiers of leadership. In 2023 we expect to see familiar faces move about the sector – public servants will transition into the private sector, and some from the private sector will move into government. What is key is that we need new ways of thinking and an openness to innovation.
Furthermore, leaders need to deliver digital health technologies and services that have people at the centre. We believe that Aotearoa needs the appointment of a national Chief Clinical Information Officer to bridge the clinical and technical chasm, and to have greater cultural and gender diversity in leadership roles, and are excited to see this appointment in progress.

Performance measurement: the aggregate spreadsheet’s days are over
The goal of the recent significant health reforms was to provide better health outcomes for New Zealanders, regardless of postcode. The sector has largely been receptive to these changes, appreciating the need to do things differently. However, in order to harness data and turn it into actionable information, Aotearoa New Zealand’s health system needs to standardise and simplify its data and digital environment. This will lead to an enhanced ability to monitor system performance, join up clinical workflows, improve health service delivery and maximise investment.
The opportunity for Te Whatu Ora and Te Aka Whai Ora is to quantifiably demonstrate the impacts of reform changes on equity and health outcomes. This year – in both the private and public systems – the current model of operating bespoke solutions that don’t easily integrate, and the cobbling together of performance measures from disparate systems, will be acknowledged as inefficient and too slow for operational decision-making. We expect to see performance measurement mature from the current system of retrospective, day-old data – that is heavily reliant on extracts and laborious auditing – to real-time monitoring and dashboards.
In both private and public settings the need for change is being recognised, although how consolidation and standardisation to enable performance measurement plays out in the digital health market is yet to be seen. Success will be dependent on strategic decision making and investment, such as the proposed National Data Platform.
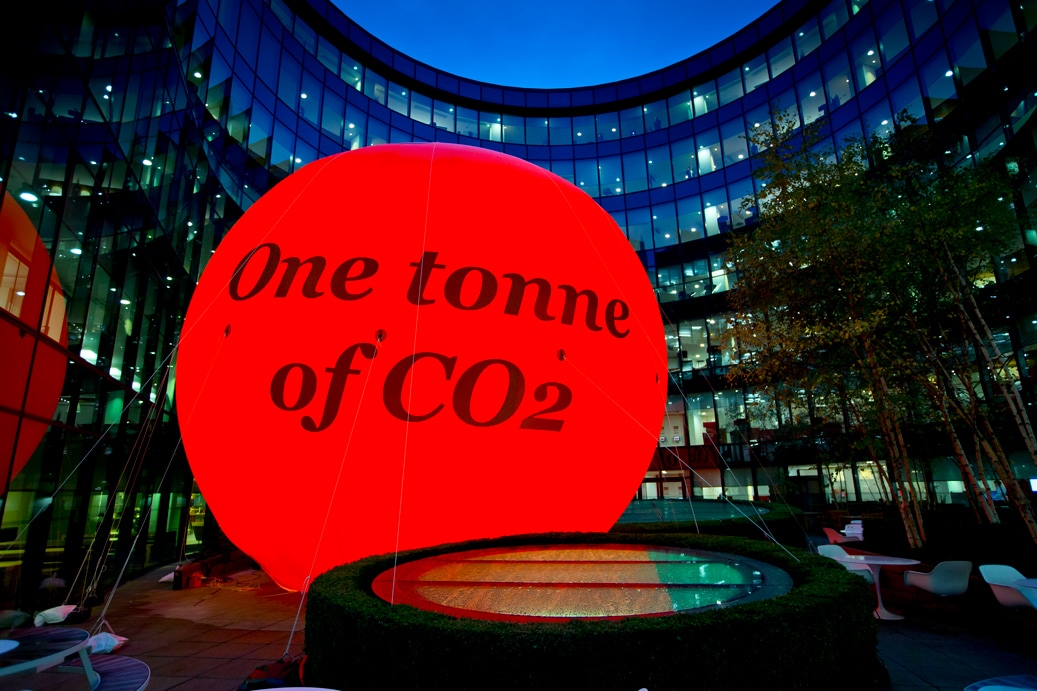
Net zero: the sector needs to cut the carbon
As recent weather events attest, Aotearoa New Zealand's climate is changing, and it is doing so in ways that impact our health. As temperatures increase so does the likelihood of tropical diseases such as dengue fever, and heat wave events can increase deaths, heat stroke, and heart and lung problems. Rising water temperatures and increased rainfall are impacting fresh and marine water resources, increasing the risk of water-related illnesses and flooding, putting pressure on systems and leaving people homeless. Those who suffer from seasonal allergies will be impacted by higher pollen concentrations and longer pollen seasons.
Addressing the health sector’s own contribution to climate change is a crucial step in reducing the impact on the health and wellbeing of people, yet the health system is the largest emitter of carbon emissions in Aotearoa New Zealand’s public sector.
New Zealand’s Carbon Neutral Government Programme has direct implications for the public healthcare sector, which is required to assess and disclose its climate change emissions and be carbon neutral by 2025.
Digital health technologies are an important enabler of the transition to net zero. Virtual appointments, self management tools and wearables, online booking and scheduling and electronic medical records contribute to reductions in greenhouse gas emissions. The transition from on-site data centre – with high energy and cooling requirements – to cloud hosting is also a key move.
The frontline digitisation of paper clinical workflows is a logical step, however there are other areas where digital transformation can deliver eco benefits. For example, the University Hospital of Morecambe Bay NHS Foundation Trust realised savings of close to $NZ50,000 of food waste annually with its patient meal ordering app.
In 2023 we will see net zero feature more prominently in healthcare discussions and the digital health community has the ability to lead by example. Adapting and mitigating climate change is possible and, by adopting omnichannel approaches to health and well-being care, will reduce inequities and increase health outcomes.
Summary
2023 is going to be a year of change, a metamorphosis of the health and wellbeing sector. Our key takeaways are:
The need for real-time performance measurement and monitoring is increasing and we need to accept that our make-do, cobbled-together systems just aren’t up to the task.
That’s going to require bold leaders unafraid of making the hard calls on what to keep, what to retire, what to standardise and when to scale.
Taking lessons from other OECD countries, we hope to see the development of an enterprise Patient Administration System, EMR, or CRM for Te Whatu Ora.
People, whānau and clinicians will get more seats at the table which will lead to more innovations in holistic health and well-being models of care.
More technology standards will support the sharing of key information across care settings.
Additional funding to enable scaling will require evidence and measurement.
International and domestic greenhouse gas emissions commitments will formally enter the digital health landscape.
About us
Our Data & Digital team brings trusted expertise to provide best practice solutions, service design, operating models and stakeholder engagement. We work with Government agencies, PHOs, public and private hospitals and providers, social sector agencies, Māori and Pacific health organisations, and industry providers.









